CHA Physician Leads Effort to Help COVID-19 Patients with Food Insecurity
At CHA, we understand how the social determinants of health (SDOH) or the conditions in which people are born, live, learn, work, play and age impact health outcomes.
Most of what keeps people healthy are circumstances outside of medical care – insufficient or poor quality food, housing, utilities, employment and education.
Recognizing the importance of these factors on health, CHA launched a program several years ago to screen for some of these conditions and connect people to resources. If patients screen positive, they receive resource sheets tailored to their language and place of residence in their After Visit Summary (AVS). These sheets were developed by a Social Determinants of Health Steering Committee and the Department of Community Health Improvement in collaboration with social service agencies and are updated on a regular basis.
If patients indicate they want help, patient resource coordinators reach out to help them navigate the system. Building on a prior pilot, if patients indicate we can share their information, we refer them directly to Project Bread, a social service agency that will help connect them to Supplemental Nutrition Assistance Plan (food stamps) and local food resources. Over the past few years, CHA has screened more than 20,000 mostly Medicaid patients for food insecurity.
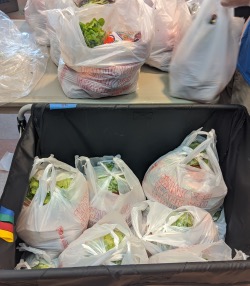
With the outbreak of COVID-19, social support systems already in place were upended, and new structures had to be formed. CHA Primary Care rapidly built a robust system to manage COVID positive/presumptive positive patients in the community. Food insecurity came up several times for patients who were COVID positive, but there was no systematic process for screening and referral for this need. In the community organizations such as Food for Free, Bread of Life, Malden YMCA, Shape Up Somerville, Maverick Community Landing Services, Community Cooks, Fresh Truck and others had quickly developed the capacity to safely meet food needs.
Primary care physician Amy Smith, MD, MPH, saw an opportunity to build on existing systems to connect COVID-19 positive patients experiencing food insecurity to these community-based organizations. She reached out to colleagues Lisa Brukilacchio at CHI and Leah Zallman, MD, MPH, from the SDOH Steering Committee, with whom she had worked on the referral process to Project Bread. Within a week COVID-19 positive patients experiencing food insecurity were flagged (with consent) and connected to the appropriate nonprofit to provide two weeks of free food aid to cover the quarantine period.
Over the past several weeks, more than 450 COVID-19 positive patients and over 1600 household members in quarantine facing food insecurity were connected with support. The project has succeeded because it built on CHI’s connections to the community, CHA’s experience with screening and referring for food insecurity, and our system for community management of COVID positive patients.
This pandemic has caused economic damage, increased food insecurity and may lead to other challenges in the coming months. If there is another surge of COVID-19 in Massachusetts, we will now be better equipped to support our food-insecure patients who need to be quarantined. Our ability to support their needs to isolate will relieve some suffering for the patient and their household members as well as addressing the public health goal of decreasing the risk of disease transmission in the community.